The Role of Preimplantation Genetic Testing (PGT) in Personalized Medicine: Tailoring IVF for Genetic Disorders
This blog explores the role of Preimplantation Genetic Testing (PGT) in personalized medicine, particularly in IVF. It covers how PGT helps tailor IVF treatments for genetic disorders, enhancing success rates and reducing the risk of inherited diseases. The article dives into different types of PGT, including PGT-A, PGT-M, and PGT-SR, and explains how advancements in genetic screening and next-generation sequencing (NGS) are shaping the future of reproductive medicine.
Gentaur
Scientific Publications
The Role of Preimplantation Genetic Testing (PGT) in Personalized Medicine: Tailoring IVF for Genetic Disorders
Introduction to Personalized Medicine in IVF
In the past few decades, the medical field has made remarkable progress in genetic research, offering more tailored and effective treatments for a variety of conditions. One of the most innovative applications of genetic testing is in In Vitro Fertilization (IVF), where Preimplantation Genetic Testing (PGT) is revolutionizing the way we approach the selection of embryos, particularly for individuals at risk of passing on genetic disorders. Personalized medicine, particularly in reproductive medicine, focuses on tailoring treatments to the individual’s genetic profile, optimizing both the chances of pregnancy and the health of the child.
Preimplantation Genetic Testing (PGT) has become an essential part of IVF by allowing for the genetic screening of embryos before they are implanted in the uterus. This testing can identify genetic abnormalities that could lead to miscarriage, congenital disabilities, or other severe health conditions. As we delve deeper into the role of PGT in personalized medicine, it is important to understand how it works, its benefits, and its transformative potential for patients undergoing IVF treatments.
Understanding Preimplantation Genetic Testing (PGT)
PGT involves screening embryos created through IVF for genetic defects. There are three primary types of PGT:
- PGT-A (Preimplantation Genetic Testing for Aneuploidy): This test identifies embryos with abnormal chromosome numbers, such as missing or extra chromosomes, which can lead to Down syndrome, Turner syndrome, or other genetic disorders.
- PGT-M (Preimplantation Genetic Testing for Monogenic Disorders): This test is used when one or both parents are carriers of a single-gene disorder, such as cystic fibrosis or sickle cell anemia.
- PGT-SR (Preimplantation Genetic Testing for Structural Rearrangements): This test is used to detect structural chromosomal abnormalities, such as translocations, inversions, and deletions, which may impact fertility or increase the risk of miscarriage.
Each of these tests plays a pivotal role in providing a clearer understanding of the genetic health of embryos and ensures that only the healthiest embryos are selected for implantation.
PGT and Personalized Medicine: A Perfect Match
Tailoring IVF Treatments Based on Genetic Risk Profiles
Personalized medicine is all about understanding the genetic makeup of an individual and tailoring treatments accordingly. For couples undergoing IVF, personalized medicine through PGT allows for the selection of embryos that carry the least genetic risk, leading to higher success rates and healthier pregnancies.
For example, couples with a family history of monogenic disorders may opt for PGT-M to screen embryos for known mutations linked to conditions like Huntington's disease or Thalassemia. This approach can be life-changing for families who would otherwise face the uncertainty of passing these conditions on to their children.
The Science Behind PGT: How It Works
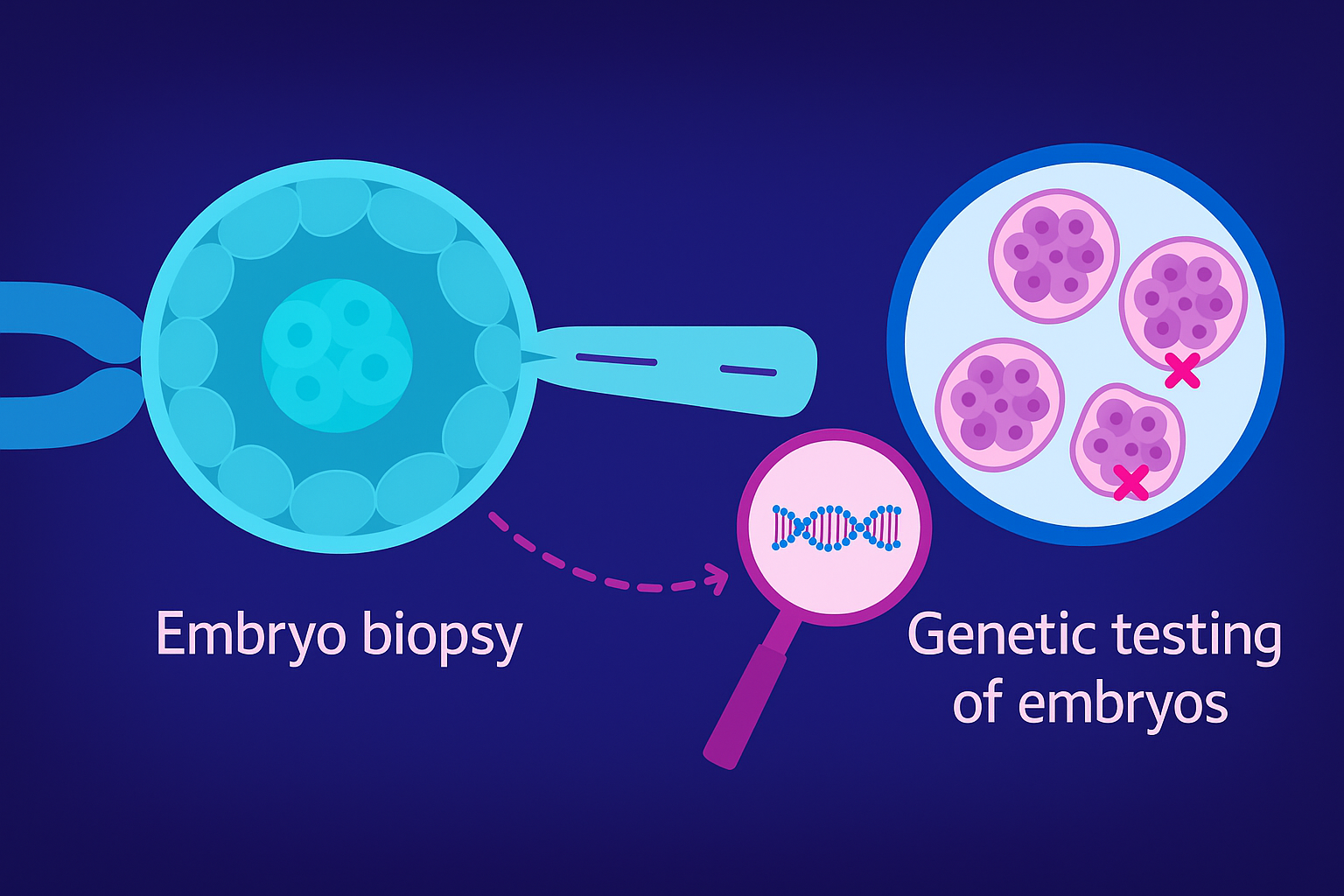
The process of PGT begins with embryo biopsy, which involves removing a few cells from the embryo (usually at the blastocyst stage). These cells are then analyzed in a laboratory to determine whether they carry genetic mutations or chromosomal abnormalities. The biopsied cells are typically analyzed using next-generation sequencing (NGS) or comparative genomic hybridization (CGH).
- Next-Generation Sequencing (NGS) allows for high-throughput sequencing of DNA, providing a comprehensive analysis of an embryo’s genetic material. It is especially useful for detecting single-nucleotide polymorphisms (SNPs), which are variations in a single nucleotide that can cause genetic diseases (NIH on NGS).
- Comparative Genomic Hybridization (CGH) is another technique used to identify chromosomal imbalances, such as deletions or duplications, that could cause developmental issues (NCBI on CGH).
This genetic testing can take place alongside IVF, allowing for the pre-implantation screening of embryos. As a result, parents can select embryos that have the best chance for a healthy life, reducing the risk of genetic diseases.
Benefits of PGT in Personalized Medicine for IVF
The integration of PGT into IVF not only enhances the selection of genetically healthy embryos but also allows for a tailored approach to fertility treatments. Here are some key benefits of this approach:
- Increased Success Rates: By selecting embryos free from chromosomal abnormalities, the chances of a successful implantation and pregnancy are significantly higher. PGT has been shown to reduce miscarriage rates by up to 50% in women over 35 (Study on PGT-A).
- Reduced Risk of Genetic Disorders: Couples at risk of passing on inherited genetic conditions can now have a better understanding of the genetic makeup of their embryos and can select embryos that are free from these disorders.
- Single Embryo Transfer (SET): The ability to select healthy embryos reduces the need for multiple embryos to be implanted, which in turn lowers the risk of multiple pregnancies, which can be associated with premature birth and other complications (CDC on IVF).
- Cost-Effective Long-Term: While PGT increases the upfront cost of IVF, it can save money in the long run by reducing the number of cycles required to achieve a successful pregnancy, thereby minimizing the need for additional treatments and interventions.
Challenges and Considerations
Despite the many benefits of PGT, there are also several challenges and considerations to be aware of. One of the most significant issues is the ethical debate surrounding genetic screening. While many support the ability to select embryos based on genetic health, others raise concerns about the potential for designer babies, where non-medical traits (such as eye color or intelligence) could be selected.
Additionally, there are limitations to the types of genetic conditions that can be tested using PGT. PGT-M can only detect genetic conditions that are known and well-documented, meaning that rare or newly discovered conditions may not be identified.
Moreover, the cost of PGT can be prohibitive for some families, as it adds to the overall expense of IVF. According to the American Society for Reproductive Medicine, the cost of PGT-A can range from $3,000 to $7,000 per cycle, depending on the technology used and the number of embryos tested (ASRM on PGT).
The Future of PGT in Personalized IVF
The future of Preimplantation Genetic Testing (PGT) lies in advancements in technology. As next-generation sequencing (NGS) and other genomic technologies continue to evolve, the ability to screen embryos for a wider range of genetic conditions will increase. The integration of artificial intelligence (AI) into genomic testing will also enhance the ability to predict genetic risks more accurately.
In addition, gene editing technologies such as CRISPR may one day allow for the direct modification of embryos to correct genetic disorders before implantation, further enhancing the potential of personalized medicine in IVF (CRISPR in IVF).
Conclusion
Preimplantation Genetic Testing (PGT) is already a critical component of personalized medicine in the context of IVF. It allows for the selection of the healthiest embryos based on genetic testing, reducing the risk of passing on genetic disorders and improving the chances of a successful pregnancy. As the technology behind PGT continues to advance, it will undoubtedly play an even more pivotal role in the future of reproductive medicine, offering couples a way to have genetically healthy children while reducing the burden of inherited diseases.
Incorporating PGT into IVF is one of the most significant innovations in reproductive medicine, providing a comprehensive, genetic-based approach to fertility treatments that aligns perfectly with the principles of personalized medicine.
For more information on the science and research behind PGT, check out these resources:
Tags
- Preimplantation Genetic Testing (PGT)
- Personalized Medicine in IVF
- PGT for Genetic Disorders
- IVF and Genetic Screening
- PGT-A (Preimplantation Genetic Testing for Aneuploidy)
- PGT-M (Preimplantation Genetic Testing for Monogenic Disorders)
- PGT for Inherited Diseases
- Next-Generation Sequencing (NGS) in IVF
- Genetic Testing in IVF
- Embryo Genetic Screening
- Gene Editing in IVF
- CRISPR and IVF
- PGT in Reproductive Medicine
- IVF Success Rates and Genetic Screening
- Preimplantation Genetic Diagnosis (PGD)
- Single Gene Disorder Screening in IVF
- PGT and Chromosomal Abnormalities
- Genetic Testing for Healthy Embryos
- PGT and Ethical Considerations
- PGT IVF Benefits
- Embryo Biopsy for Genetic Testing
- Aneuploidy Screening in IVF
- IVF with Genetic Testing for Diseases
- Personalized IVF Treatments
- Genetic Screening Technologies in IVF
